Indice del volumen Volume index
Comité Editorial Editorial Board
Comité Científico Scientific Committee
FUROSEMIDE TEST: ITS PATTERN IN NOT SEVERE
CHRONIC RENAL DISEASE
Carlos G. Musso1, Soledad Crucelegui1, Juliana Reynaldi1, Bernardo Martinez2, Carolina Aparicio1, Manuel Vilas1, Luis Algranati1.
1Nephrology 2and Internal Medicine Divisions.
Hospital Italiano de Buenos Aires. Argentina
carlos.musso @ hospitalitaliano.org.ar
Rev Electron Biomed / Electron J Biomed 2008;3:40-43.
Comment of the reviewer Javier Lavilla, MD. PhD. Nephrology Department. Clínica Universitaria. Pamplona. España
Comment of the reviewer Jesús Garrido, MD. Unidade de Nefrologia e Diálise. Hospital São Teotónio de Viseu. Viseu. Portugal.
SUMMARY
Furosemide test is a simple and useful test of renal physiology used to evaluate the capability of the collecting tubules to secrete potassium under the effect of serum aldosterone. Its behaviour pattern has already been established in children and young adults but not described in chronic renal disease patients yet, which we explored in this study.
Material & Method: Twenty-six young volunteers (between 20 and 40 years old), chronically on a low potassium diet (40 mmol of K day) were studied: twenty of them were healthy young ( they were neither suffering form diseases nor on any medication), and the rest were young patients suffering from stage II / III chronic renal disease (damaged kidney with GFR between 83.1 ml-min to 39.2 ml-min) secondary to glomerular diseases documented by kidney biopsy. None of the studied chronic renal disease patients were suffering from diabetes mellitus, urinary obstruction, nor treated with dyskalemia generating drugs, such as: diuretics, angiotensin converting enzyme inhibitors, angiotensin receptor antagonists, etc. Before, while the test was being carried out and after 180 minutes of a single dose of intravenous furosemide (1 mg/kg), urine and blood samples were obtained, for creatinine and potassium levels. From these data we calculated fractional excretion (FE) of potassium. Statistical analysis was performed applying Student´s t-test.
Results: There was no significant difference neither in pre-furosemide (basal) and post-furosemide average FE of potassium between the healthy and chronic renal disease (CRD) group: 16.4 ± 8.6% (CRD) vs 11.5 ± 4.6% (healthy) (p = NS) ; 40.8 ± 3.2 % (CRD) vs 35.4 ± 8.9% (healthy) (p = NS) respectively. Conversely, there was a significant difference in post-furosemide peak FE of potassium value, which was higher and delayed in the CRD group compared to the healthy one: 49.5 ± 8.2 % at 118 mins (CRD) vs 31.6 ± 11% at 30 mins (healthy) (p = 0.001).
Conclusion: Furosemide test showed a significantly higher and delayed peak post-furosemide FE of potassium value in young chronic renal disease patients compared to healthy young people.
KEY WORDS: furosemide test, chronic renal disease, potassium
RESUMEN
El test de furosemida consiste en una prueba de fisiología renal que se utiliza para evaluar la capacidad de los túbulos colectores para secretar potasio. Dicho estímulo está mediado por acción de la hormona aldosterona , cuyos niveles séricos se elevan tras el suministro de furosemida. Si bien el patrón de respuesta de este test ha sido descrito en niños y jóvenes sanos, no se lo ha hecho aun en pacientes portadores de insuficiencia renal crónica. Por este motivo se decidió realizar el siguiente estudio a fin lograr su descripción.
Material y Método: Se estudiaron veintiséis voluntarios jóvenes (edad: 20 - 40 años), sometidos a una dieta baja en potasio (40 mmol de potasio/día): veinte de ellos eran jóvenes sanos (no presentaban ninguna enfermedad ni tomaban ninguna medicación), y el resto eran pacientes jóvenes portadores de enfermedad renal crónica estadío II/III (filtrado glomerular (FG) entre 83,1 ml/min - 39,2 ml/min) secundaria a glomerulopatía (diagnóstico por biopsia renal). Ninguno de los pacientes estudiados era portador de diabetes mellitus, obstrucción urinaria, ni estaban en tratamiento con drogas potencialmente inductoras de diskalemia: diuréticos, inhibidores de la enzima convertidora, y antagonistas del receptor de angiotensina II. Desde el comienzo del test y hasta 180 minutos post recibir una dosis única de furosemida endovenosa (1 mg/kg), se obtuvieron muestras de orina y sangre para medir niveles de creatinina y potasio. A partir de estos datos se calculó la excreción fraccional de potasio (EFK) correspondiente a cada muestra. El análisis estadístico fue realizado aplicando el test de Student.
Resultados: Si bien no hubo diferencia estadísticamente significativa ni en el valor basal (pre-furosemida), ni promedio (post-furosemida) de la EFK, entre los sujetos sanos y los pacientes con insuficiencia renal crónica (IRC): EFK basal 16,4 ± 8,6% ( IRC) vs 11,5 ± 4,6% (sanos) (p= NS); EFK promedio 40,8 ± 3,2% (IRC) vs 35% (sanos) (p= NS) respectivamente. Sin embargo, se observó una tendencia a que estos valores fueran más elevados en el grupo con IRC.
Por el contrario, si se documentó diferencia estadísticamente significativa en el pico de EFK post-furosemida, el cual fue más alto y tardío en el grupo con IRC, comparado con el sano: 49,5% ± 8,2% a los 118 min ( IRC) vs 31,6 ± 11% a los 30 min (sanos) (p= 0,001).
Conclusión: El test de furosemida mostró un mayor y más tardío pico de EFK post furosemida en pacientes jóvenes con enfermedad renal crónica en comparación con el pico de EFK logrado por los jóvenes sanos.
PALABRAS CLAVE: Test de furosemida, enfermedad renal cronica
INTRODUCTION
Furosemide test is a very simple and useful renal physiological test that evaluates the ability of the collecting tubules to secrete potassium induced by serum aldosterone secretion secondary to furosemide infusion1, 2. Its pattern in healthy children and young persons has already been described, but it has not been defined in chronic renal disease young patients who are an important target to study this test, because it is known that the renal physiology differs in the chronic renal disease people compared to the healthy young ones3-6, we hypothesized that perhaps the furosemide test could have a modified pattern in chronic renal disease people, and in this study we investigated the behaviour pattern of this functional test in a stage II / III nephropathy group.
MATERIAL AND METHODS
Twenty six young (between 20 and 40 years old) volunteers on low potassium diet (40 mmol of K day) were studied. Twenty of them were healthy and, they were neither suffering from diseases nor taking any medication, and the rest were patients suffering from stage II / III chronic renal disease (damaged kidney with GFR between 83.1 ml-min to 39.2 ml-min) secondary to glomerular diseases documented by kidney biopsy: in order to avoid including patients suffering from severe tubular-interstitial damage, and consequently with tubular resistance to aldosterone.
In each studied group, patients with different levels of GRF were incorporated in order to make each of them more representative of its corresponding stage of CRD. None of the studied chronic renal disease patients were suffering from diabetes mellitus, urinary obstruction, nor treated with dyskalemia generating drugs, such as: diuretics, angiotensin converting enzyme inhibitors, angiotensin receptor antagonists, etc.
All volunteers gave their consent to undergo a furosemide test. It consisted of the following protocol: At eight a.m. a basal blood and urinary sample (time zero) were taken from a fasting volunteer, and after that a single dose of intravenous furosemide (1mg/kg) was administered. Then, a sample was taken from every micturation until the test ended at 180 minutes. Blood samples were also taken pre-furosemide administration (time zero), and post-furosemide, at 90 and 180 minutes (end of the test). Blood pressure was also measured throughout the test every 30 minutes. The levels of potassium and creatinine were measured from the obtained blood and urinary samples in order to calculate fractional excretion of potassium values: we obtained the basal value (pre-furosemide infusion: time zero), the average post-infusion value (the mean value of the post-furosemide samples), and the peak value (highest value post-furosemide infusion).
Fractional excretion of potassium (K) was calculated applying the following formula (3): (urinary K / plasma K) x (plasma creatinine / urinary creatinine) x 100
All individuals remained fasting during the duration of the test. At the end of the test, in order to avoid complications secondary to dehydration, the amount of urine volume passed was replaced, half of it intravenously (normal saline) and the rest with tap water per os.
Statistical analysis was performed applying Student´s t-test, since the normality pattern of the obtained data was very hard.
None of the volunteers had any contraindication to participate in a furosemide test, such as hypotension, hypokalemia, dehydration or allergy to furosemide and sulfas, and they signed a consent form approved by the Hospital´s Institutional Review Board.
RESULTS:
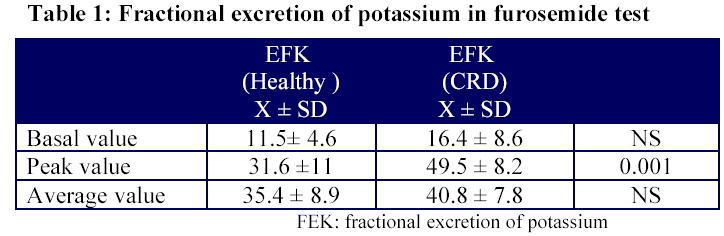
There was no significant difference neither in pre-furosemide (basal) and post-furosemide average FE of potassium between the healthy and chronic renal disease (CRD) group: 16.4 ± 8.6% (CRD) vs 11.5 ± 4.6% (healthy) (p = NS) ; 40.8 ± 3.2% (CRD) vs 35.4 ± 8.9% (healthy) (p = NS) respectively (Table 1). However, the above mentioned FE of potassium values (basal and average) showed a trend to be a 5 % higher in CRD patients compared to healthy people.
Finally, there was a significant difference in post-furosemide peak FE of potassium value, which was higher in the CRD group compared to the young one: 49.5 ± 8.2% (CRD) vs 31.6 ± 11% (healthy) (p = 0.001) (Table 1).
Regarding post-furosemide fractional excretion of potassium peak value, it was reached delayed in CRD group compared to the healthy one: at 118 mins vs 30 mins respectively.
The documented nephropathies in the CRD group were: IgA (n: 4), membranous (n: 1) and membranoproliferative (n: 1) glomerulonephrities.
DISCUSSION:
Even though, it was not found a significant difference between the groups respect to the basal (pre-furosemide) fractional excretion of potassium: 16.4 ± 8.6 (CRD) vs11.5 ± 4.6 (healthy), and post-furosemide average FE of this cation: : 40.8 ± 3.2% (CRD) vs 35.4 ± 8.9% (healthy), both indexes showed to be a 5% higher in the CRD group compared to the healthy one. Perhaps, the low number of CRD volunteers enrolled in this study was not enough in order to detect an statistically significant difference in this sense.
Conversely, the post-furosemide peak fractional excretion of potassium was significantly higher in the CRD patients compared to the healthy one (Table 1).
Furthermore, the difference between peak and basal FE of potassium was around three times in both groups: 3 times (nephropathy) and 2.8 times (healthy).
Urinary potassium excretion is increased post-furosemide infusion in the healthy young, primarily because of the increase in sodium delivery, to the collecting tubules which stimulates sodium reabsorption, electronegative luminal charge and consequently potassium secretion. Besides, furosemide also increases urinary potassium secretion by inducing a hypovolemic state which stimulates aldosterone release and consequently potassium secretion7-8.
The finding of a trend to a 5% increase in basal and average FE of potassium, as well as a significant augment in peak FE of this cation in the studied CRD group compared to the healthy people one, could be explained by the pre-furosemide higher FE of potassium values in chronic nephropathy which is a phenomenon secondary to the classical compensatory augment in tubular potassium secretion capability described in this sort of patients. The above described phenomenon is induced by the aldosterone hormone, since its elevated serum levels in chronic nephropathy, stimulates renal potassium secretion, allowing them to keep normal serum potassium levels until GFR higher than 10 ml-min3-6.
Finally, the post-furosemide peak fractional excretion of potassium was reached later in the CRD people (at 118 mins) compared to healthy one (30 mins). Perhaps, the kidney condition of damaged organ in CRD could explained why even though it is able to achieve an adequate potassium secretion response, it is also a delayed one.
One of the main limitations of this study was the low number of volunteers (n: 6) enrolled in the CRD group. However, this was a direct consequence of incorporating in this group just those ones who were not suffering from severe tubular-interstitial histological damage, because of its importance in the tubular response to aldosterone.
Besides, even though pharmacokinetics of furosemide is different between healthy people and chronic renal disease patients: prolonged half-life and extra-renal clearance of furosemide in chronic nephropathy, etc., our objective was just to describe the normal patter of furosemide test ( FEK peak value and time) in chronic renal disease patients, where it was not described yet, beyond the reason that explains this response.
CONCLUSION: Furosemide test showed a significantly higher (50%) and delayed (120 minutes) peak post-furosemide FE of potassium value in stage II - III chronic renal disease young patients compared to healthy young people.
REFERENCES
- 1.-Rodriguez Soriano J, Vallo A. Los diureticos como metodo de estudio de la funcion renal. Nefrologia. 1990; 1: 44-50.
2.- Rose B, Post T. Uso clínico de los diuréticos. In Rose B, Post T (Eds). Transtornos de los electrolitos y del equilibrio ácido.base. Madrid. Marbán. 2002: 447-477.
3.- Swartz R. Fluid, electrolyte, and acid-base changes during renal failure. In Kokko J, Tannen R (Eds). Fluids and electrolytes. Philadelphia. W.B. Saunders Company. 1996: 487-532.
4.- Musso C, Liakopoulos V, Stefanidis I, De Miguel R, Imperiali N, Algranati L. Correlation between creatinine clearance and transtubular potassium concentration gradient in old people and chronic renal disease patients. Saudi J Kidney Dis Transpl. 2007; 18(4): 551-5.
5.- Musso , Liakopoulos V, De Miguel R, Imperiali N, Algranati L. Transtubular potassium concentration gradient: comparison between healthy old people and chronic renal failure patients. Int Urol Nephrol. 2006; 38(2):387-90.
6.- Musso CG, Miguel R, Algranati L, Farias E. Renal potassium excretion: comparison between chronic renal disease patients and old people. Int Urol Nephrol. 2005; 37(1): 167-170.
7.- Lacy C, Armstrong L, Goldman M, Lance L. Drug information handbook. Hudson. Lexi-Comp. 2004: 697-699.
8.- Halperin M, Goldstein M. Potassium physiology. In Halperin M, Goldstein M (Eds). Fluid, electrolyte, and acid-base physiology. Philadelphia. WB Saunders Company. 1999: 371-400.
Received: September 17, 2008. Received reviewed: December 11, 2008
Published: December 30, 2008.
