Indice del volumen Volume index
Comité Editorial Editorial Board
Comité Científico Scientific Committee
UTERINE ARTERY EMBOLIZATION FOR THE TREATMENT OF UTERINE FIBROIDS.
Ángel García-Iglesias1, Santiago González Perez
2,
David Beltrán Vaquero3, María de la O
Rodríguez Martin1,
Silvia García Valle4, José Luis Pérez Escanilla1,
María José Doyague Sánchez1, Jesús García Alonso2,
Luis Velasco Pelayo2, Josefina Basabe Picaso1
1Obstetric and Gynecology, 2Interventional Radiology Departments.
Universitary Hospital of Salamanca. Spain
3Institute of Public Health of Madrid.
4Pharmaceutical. Master's degree in Toxicology. Madrid.
Spain
aiglesias @ usal.es
Rev Electron Biomed / Electron J Biomed 2013;1:9-17.
Comment of the reviewer Dra. Beatriz Cuevas Ruiz MD. PhD. Servicio de Hematología y Hemoterapia. Hospital Universitario de Burgos. Spain
Comment of the reviewer Carlos G. Musso, MD. PhD.
Ageing Biology Unit. Hospital Italiano de Buenos Aires. Argentina
ABSTRACT
AIM: To determine the outcome of uterine artery embolization in patients with symptomatic uterine fibroids, in order to assess the response of symptoms and fibroid size.
METHODS: We analyzed the results of a population study of 112 patients with uterine fibroids made in the period between 2006 and 2010. Main parameters were assessed improvement or disappearance of symptoms and downsizing the adverse effects of the procedure.
RESULTS: The predominant age of the patients are in the group of 41-45 years with 80.35%, being the most common symptom of menorrhagia 66.07%, myoma volume ranged between 35cm3 and 523cm3, and procedure duration ranged from 1 hour to 2.5 hours. The most common symptoms after embolization was mild pain 44.64%, not having symptoms in 43.75%. Also it was associated nausea in 8.03% and vomiting in 3.57% as other adverse effects. After three months of treatment 47.32% had oligomenorrhea and amenorrhea was 17.85%. Fibroid size at 6 months was reduced significantly dominate the volume between 36 and 113cm3.
CONCLUSION: Uterine artery embolization is an effective treatment for symptomatic fibroids, considered an alternative to surgical treatment.
Key words: syntomatic myomas, leiomiomas, uterine artery embolization.
RESUMEN: EMBOLIZACIÓN DE LAS ARTERIAS UTERINAS PARA EL TRATAMIENTO DE FIBROMAS UTERINOS.
OBJETIVO: determinar el resultado de embolización de la arteria uterina en pacientes con fibromas uterinos sintomáticos, con el fin de valorar la respuesta de los síntomas y el tamaño de los miomas.
MÉTODOS: Se analizaron los resultados de un estudio que incluye 112 pacientes con fibromas uterinos, estudiadas y tratadas en el periodo entre el año 2006 y 2010. Los parámetros principales evaluados fueron: la mejoría o desaparición de los síntomas, la reducción del tamaño y los efectos adversos del procedimiento.
RESULTADOS: La edad predominante de las pacientes está en el grupo de 41-45 años representando el 80,35%, y siendo el síntoma más común la menorragia, presente en el 66,07% de las mujeres incluidas en el estudio. El volumen de los miomas osciló entre 35cc y 523cc, y la duración del procedimiento fue de 1 hora a 2,5 horas. El síntoma más común después de la embolización, consistió en un dolor leve referido por el 44,64% de las mujeres, frente a un 43,75% que permanecieron asintomáticas. También se registraron náuseas y vómitos en el 8,03% y en el 3,57% respectivamente, como efectos adversos al procedimiento. Transcurridos tres meses del tratamiento, el 47,32% presentaron oligomenorrea y un 17,85% amenorrea. El tamaño del mioma a los 6 meses tras la embolización de la arteria uterina se redujo de forma significativa, disminuyendo el volumen entre 36 y 113cc.
CONCLUSIONES: La embolización de la arteria uterina es un tratamiento efectivo para los miomas sintomáticos, representando una alternativa al tratamiento quirúrgico. Palabras clave: miomas sintomáticos, leiomiomas, embolización de la arteria uterina
INTRODUCTION
Uterine fibroids, or myomas, are tumours of the smooth muscle layer of the uterus, which appear in approximately 25% of all fertile women. Although some of these fibroids are asymptomatic, more than 50% of them cause symptoms that require treatment. Some of the most common symptoms are metrorrhagia, anemia or compressive symptoms, such as pain or mass effect, which also have a large influence on fertility1.
Treatment of fibroids presents several alternatives, from medical treatments with hormones (levonorgestrel) and gonadotropin-releasing hormone analogues (GnRH analogues), to surgical treatments, which have been for many years the most used therapeutic approach. The most commonly techniques used were hysterectomy or myomectomy, either by laparotomy or laparoscopy, together with the hysteroscopic resection of the fibroid2. However, the combination of risks associated to surgical treatments and the effects that surgery sometimes has on young women, which can sometimes affect or hinder fertility, together with the fact that patients wish to avoid surgery3 have led to the search of alternatives for surgical approaches. Embolization appears as an alternative for traditional therapies for patients with symptomatic fibroids.
This approach is adequate in premenopausal patients who wish to avoid hysterectomy or who present medical contraindications for surgery4. Ravina5 initially developed the embolization of fibroids in France. Afterwards, in 1997, the results for patients treated in the USA were published6.
Our objective is to present the results of uterine artery embolization on women with symptomatic uterine fibroids.
MATERIAL AND METHODS
Observational, multi-center and retrospective study.
Study population:
We analyzed the results of 112 uterine artery embolization procedures carried out in the Unit of Interventional Radiology of the University Hospital of Salamanca on patients who were transferred from the external consultations of the Department of Gynecology and also from other centers, who were diagnosed with intramural uterine fibroids and presented symptoms such as metrorrhagia, anemia and/or mass effect. Patients who were allergic to iodinated contrasts were excluded from the study.
Exclusion criteria were fibroid tumors of more than 12 cm, subserosal fibroids and submucosal fibroids. Desire for fertility was a partial exclusion criterion. Before the embolization, a Nuclear Magnetic Resonance (NMR) was performed in order to define the location, size and number of tumors. Analysis, pregnancy test and hormonal study were also carried out.
All the patients received written information about the treatment they would undergo, together with its alternatives and the informed consent form.
Procedure
All patients were scheduled for hospitalization. Urinary catheterization and the insertion of a peripheral intravenous catheter were established as compulsory steps before the procedure.
Analgesia was provided by the Department of Anaesthetics with the insertion of an epidural analgesia catheter that was kept for at least 24 hours. Antibiotic prophylaxis with cefazolin 2g was also provided one hour before the procedure.
The most common approach for the uterine artery embolization is the right common femoral artery. The procedure generally starts with the Seldinger technique (the needle and the guide-wire are placed in the sheath and the catheters pass through it). The common femoral artery is punctured, generally on the right side, but in some cases also bilaterally, with an Abbocath catheter 18G and a 0.35" radioscopically guided hydrophilic guide-wire. Then, the 4-F or 5-F size Cobra, Multipurpose and reverse Simmons selective catheters pass through it, with a cross-over and Waltman loop technique for the corresponding catheters of the hypogastric artery and the identification of the uterine arteries from both sides, with the adequate radiological projections. In some cases, an aortoiliac angiography with a pigtail catheter is performed before this stage, but it increases the exploration time and the radiation dose. It is advisable to leave the 4-F or 5-F catheter in the hypogastric artery and to use road-mapping for the catheterization, with a coaxial micro-guide and a 3-F micro-catheter in the uterine artery, in order to avoid spasms that would prevent embolization. The catheters will surpass the point of exit of the cervico-vaginal arteries.
Once in the last horizontal or ascending portion of the uterine artery, 1-3cm syringes are used to administer antegrade injections of PVA (polyvinyl alcohol) particles of 300-500 microns and then 500-700 microns, or embospheres of 500-700 and 700-900 microns, pre-loaded with physiological saline solution and contrasts with a medium concentration of 50%. Our objective is to close the arterial input of the fibroid, because its tissue is highly sensitive to ischemia. Thus, we can maintain a normal endometrial and myometrial vascularization, that is, the vessels of the perifibroid plexus are occluded while the uterine perfusion is maintained.
The end-point is randomly determined after the fibroma is devascularized, with a retrograde flow towards the internal iliac artery or a slow antegrade pump flow of 5 beats.
At the end, the common femoral artery is compressed by hand, or sealed with devices for percutaneous closure.
During the procedure, some radioprotection measures were applied, such as a minimal magnification, the collimation of the fluoroscopic image, short series of images per second and anteroposterior projection. The monitoring of a potential post-embolization syndrome is carried out in the recovery room and in the section of gynecology. The monitoring process lasted for 24-48 hours.
Statistical study
The clinical characteristics were evaluated statistically by use of the Fisher's exact or Chi-square test with linear by linear association. Statistical analyses were undertaken using SPSS software (version 18). A P-value <0.05 was considered statistically significant.
RESULTS
The age of the patients ranged between 29 and 50 years. The 29-year-old patient presented a 10cm fibroid tumor, and she wanted to keep her uterus, so she asked for an embolization, because surgery involved a myomectomy and it could not guarantee its integrity. Two patients included in the group between 31 and 35 years old also wanted to keep their uteruses intact. The largest group included patients between 41 and 45 years, with 90 patients (80.36%), followed by the group of patients between 46 and 50 years (16 patients, 14.28%). They all met the criteria for embolization. The main symptom for consultation was menstrual alterations with menorrhagia (66.07%), followed by metrorrhagia (19.65%) and polymenorrhagia (14.28%). All the patients presented anemia and had a long-duration treatment for iron deficiency. They all underwent an ultrasound study in which the presence of one or more fibroids was established (Table 1).
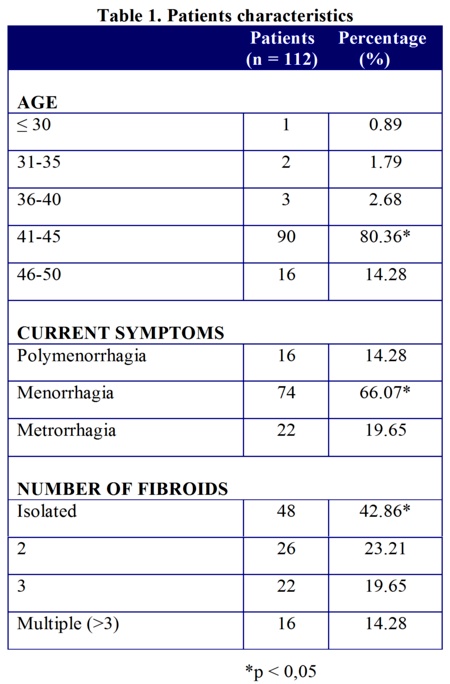
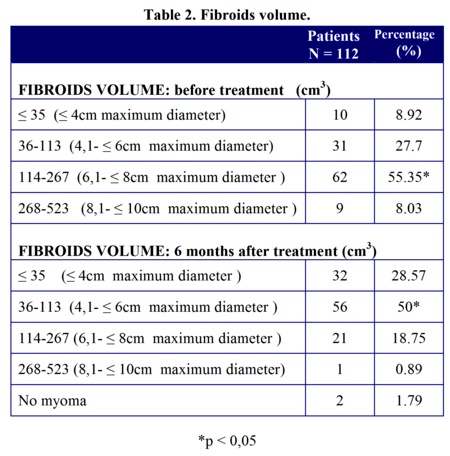
There was a single tumour in 42.86%; 23.21% presented two tumors; 19.65% presented three tumours; and 14.28% had a polyfibroid uterus. The volume of the fibroids was confirmed by NMR and it ranged between <35cm3 and 523 cm3. In 8.03%, the fibroids reached a volume of 268cm3 and 523 cm3, while the tumors most commonly subject to embolization had a volume between 114cm3 and 267cm3 in 55.35% of the treated fibroids. In 27.7%, the fibroids had a volume between 36 cm3 and 113 cm3, and 8.92% had fibroids of less than 35cm3 (Table 2).
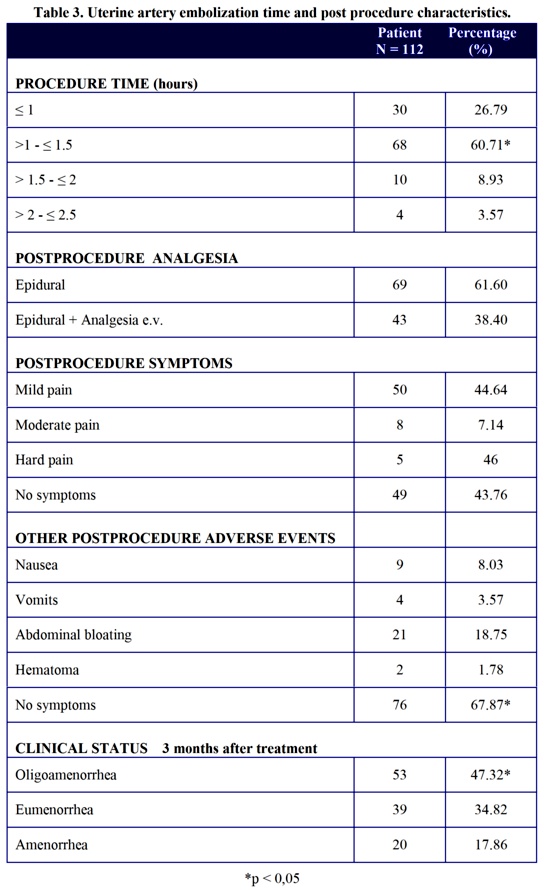
The duration of the embolization procedure was highly variable, depending on multiple factors, such as size, location and the presence of cesarean scars or scars due to other type of operations, ranging from 2 hours (>1.5 - <2h) (8.93%), to 1 hour 30 minutes (>1 - <1.5h) (60.71%) and to 1 hour (<1h) (26.79%).
The uterine artery embolization involves the appearance of ischemia, which manifests itself as pain. All the patients were treated with analgesia, via a catheter for the first 24 hours, and then with intravenous and oral analgesia. The pain was hard in 4.46%, moderate in 7.14% and mild in 44.64%. 43.76% did not present any pain.
Apart from pain, other types of clinical alterations can appear during the immediate period after embolization. The most important one was abdominal bloating or distension (18.75%), nausea (8.03%) and vomiting (3.57%). 67.87% did not present any of these symptoms.
Six months after embolization, menstruations had changed in all cases. 47.32% presented oligomenorrhea; 34.82% presented normal menstruation (eumenorrhea); and 17.86% presented amenorrhea, which could be helped by the age of the patient, her hormonal condition and the size of the fibroid tumor. (Table 3).
Six months after embolization, the volume of the tumor had been reduced at different degrees. In 28.57% of the patients, it was equal to or smaller than 35cm3; in 50% of the patients, the volume was between 36cm3 and 113cm3; and in 19.04% of the patients, it had become calcified. Table 2.
Analgesia was provided with catheter along in 61.60%, and with catheter plus intravenous analgesia in 38.40%.
DISCUSSION
The use of an alternative technique to surgery with a lower morbidity and shorter hospital stays represents a significant medical advance, because women who do not wish to undergo a hysterectomy for a fibroid tumor have now access to different less-invasive alternatives7.
The embolization technique involves a selective blockade of the blood flow of the vessels of the fibroid with embolic agents through catheters. These embolic agents can be classified into different types8, 9, 10, and the literature does not describe any problems related to any possible reactions they might cause. The insertion of catheters does not require general anesthesia, and it can be done with local anesthesia and a mild sedation11, although the insertion of an epidural catheter allows for a proper analgesia and the control of pain after the embolization.
The size of the fibroids that underwent embolization was variable, although they were usually of less than 10 cm. The effectiveness of the embolization of giant fibromas has been assessed, and a total reduction has been observed in 42.9% of the cases12. The results described after embolization are very similar.
It was evaluated efficacy of embolization of the uterine arteries in uterine myomas depending on peculiarities of the blood flow in the system of the uterine arteries reports very positive results, and in the points out a prolonged irritation of the puncture site as the most common adverse effect reported by the patients13. The most favorable finding was the immediate remission of the symptoms. Sone10 reports the remission of menorrhagia in 90% of the cases, of the pelvic pain in 78% of the cases, of the general symptoms in 98% of the cases and a reduction of the volume of the fibroid after 12 months in 61% of the cases. He used gelatin sponge for the embolization. A comparative study14 was carried out with 375 patients with symptomatic fibroids who underwent different treatments (embolization, myomectomy and hysterectomy). 12 months after treatment, the three procedures had resolved the symptoms, and hysterectomy was the most effective approach for the resolution of the clinical disorder. Embolization was the technique with the best recovery rates regarding time and low morbidity. Apart from the symptoms, the reduction of the size of the uterine fibromas is another important aspect to be taken into account. A study reports a volume reduction of 50% after one year and all patients were asymptomatic15.
One of the circumstances to be considered is the state of the endometrium and the uterine muscle. The NMR revealed a transient ischemia of the uterus which involved the endometrium and the lower and middle part of the myometrium of the uterine body and the fundus of the uterus. However, no alterations are found in the cervix and the subserosal tissue. In most cases, the myometrial tissue recovers completely after 48-72 hours, while the fibroid tumor suffers an irreversible infarction due to the ischemia16. In the diagnosis of fibroids and the monitoring after embolization, ultrasounds and NMR can be safe and reliable techniques. However, comparative studies have revealed some differences in the volume of the tumors between both techniques and NMR has been more effective in the characterization of fibroids16, 17, and the monitoring after embolization can be carried out with ultrasounds18.
Possibly, one of the problems derived from the different treatments of fibroid tumors can be due to the choice of the technique. Therefore, the alternatives for any single approach must be also taken into account. A study assessed the response after 5 years for two randomly distributed groups of patients who underwent hysterectomy and embolization. In the patients who underwent embolization, 24.7% had also underwent a hysterectomy because the symptoms had not completely disappeared, which reveals that embolization can be an alternative for hysterectomy and, with a proper selection of indications, can produce very positive results. For this reason, it is crucial to adequately select the patients and to define the location and size of the tumor, which are essential factors for good results19. A study compared the effectiveness, feasibility and morbidity rates of preoperative embolization or ligature of the uterine arteries in the preparation for conservative surgery of uterine fibroids, in which the choice of approach depends on the amount, size and topography of the fibromas20. These techniques are effective in the reduction of bleeding and they are compatible with fertility. With regard to the adverse effects they can present, a study shows the appearance of pre-menopausal symptoms or the appearance of menopause21 and the spontaneous vaginal expulsion of the fibroid22.
There are some doubts about the possibility that patients who underwent an embolization may present ovarian cancer, but at the present moment there are no published studies or references on the subject23. However, one case of advanced ovarian carcinoma after an embolization has been described24.
The most complex situation derived from embolization is the preservation of fertility. There are few publications related to the problems of pregnancy after embolization, although they indicate that some of the pregnancies go on to term, albeit with an increased number of miscarriages and preterm deliveries. A study that monitored 100 patients who underwent embolization with tris-acryl gelatin microspheres detected 11 pregnancies (19.2%) of all patients who wished to preserve their fertility), with 8 live birth (4 of them with vaginal birth and 4 of them with a Cesarean section). Gestation lasted for approximately 37 weeks and none of the fetuses showed chromosomal abnormalities. No abnormal placental implantations were observed25. However, a study showed the appearance of placenta accreta in women who underwent embolization of a fibroid tumor and got pregnant afterwards26.
As a conclusion, the embolization of the fibroid tumor can be an effective alternative for the resolution of symptoms (particularly anemia) caused by these benign tumors without the need of surgery.
ACKNOWLEDGEMENTS: We would like to thank secretaries Mrs. Mari-Humi and Mrs. Amalia, and the Assistant Medical Director, Dra. P. Reyes for support in the implementation of this technique.
DISCLOSURE OF POTENTIAL CONFLICTS OF INTEREST: The authors declare that there is no conflict of interest in the present study
REFERENCES
1.-Aubuchon M. Pinto A. Wilians DB. Treatment of uterine fibroids. Obstet Gynecol. 2002;9(6):231-237.
2.-Dutton S. Hirst A, McPherson K, Nicholson T, Maresh M. A UK multicentre retrospective cohort study comparing hysterectomy and uterine artery embolisatiom for the treatment of syntomatic uterine fibroids (HOPEFUL study) main results on medium-term safety and efficacy. BJOG 2007;114 (3):1340-1351.
3.- Helal A, Mashaly A, Amer T. Uterine artery occlusion for treatment of symptomatic uterine myomas. JSLS 2010;14 (2)386-390.
4.- Volkers NA, Herenkampt WJ, Birnie E, De Vries C, Holt C, Ankun WM et al. Uterine artery embolization in the treatment of symptomatic uterine fibroid tumors: periprocedural results and complications. JVIR 2006;17 (3):471-480.
5.-Ravina JH, Herbreteau D, Ciraru-Vigrneron N, Bouret JM, Houdart E, Aymard A, et al. Arterial embolization to treat uterine myomata. Lancet 1995; 346(4W):671-672.
6.- Goodwin SC, Vedantham S, McLucas B, Forno AE, Perella R. Preliminary experience with uterine artery embolization for uterine fibroids. JVR 1997;8 (5):517526.
7.- Stovall DW. Alternatives to hysterectomy focus on global endometrial ablation uterine fibroid embolization and magnetic resonance-guided focused ultrasound. Menopause 2011,18 (4):437-444.
8.- Bihim T, Pisco JM, Duarte M, Oliveira AG. Polyvinyl alcohol particle size for uterine artery embolization: a prospective randomized study of initial use of 350-500 um particles. J Vas Interv Radiol 2011; 22(1):21-27.
9.-Lohle PN, De Vries J, Klazen CA, Boekkooi PF, Vervest HA, et al. Uterine artery embolization for symptomatic adenomyosis with or without uterine leiomyomas with the use of calibrated tris-acryl gelatin microspheres: midterm clinical and MR imaging follow-up. J Vasc Interv Radiol 2007; 18 (7):835-841.
10.- Sone M, Aral Y, Shimizu T, Takeuchi Y, Higashihara H, Ohgi S. Et At. Phase I/II multiinstitutional study of uterine artery embolization with gelatin sponge for syntomatic uterine leiomyomata: Japan intervional radiology in oncology study group study. J Vasc Interv Radiol 2010; 21(11):1665-1670.
11.-Smith SJ. Embolization leiomyoma uterine. Am Fam Physician 2000; 61 (7):3601-3611.
12.- Nasser F, Alfonso BB, de Jesus SG, Coelho D, Ziotnik E, Messina MD. et al. Uterine fibroid embolization in women with giant fibroids. Rev Bras Ginecol Obstet. 2010; 32 (11):530-535.
13.- Mukhamed'ianov IF, Fedorov SV. Clinical aspects of uterine embolization efficacy in uterine myomas. Angiol Sosud Khir 2010; 16 (2):43-46.
14.-Spies JB, Bradley LD, Guido R, Maxwell GL, Levine BA, Coyne K. Outcomes from leiomoma therapies: comparison with normal control. Obstet Gynecol 2010;116(3):641-652.
15.- Miljailovic MZ, Lukic SM, Jankovic SM, Surlan K. Arterial embolization of uterine fibroids. J Buon 2010;15(4):704-707.
16.-Scheuring-Muernkler C, Wagner M, Franiel T, Hamm B, Kroencke TJ. Effect of uterine artery embolization on uterine and leiomyoma perfusion: evidence of transient myometrial ischemia on magnetic resonance imaging. J Vasc Interv Radiol. 2010;21(9):1347-1353.
17.- Rajan DK, Margau R, Kroll RR,Simons ME, Tan KT, Jaskolka JD. Et Al: Clinical utility of ultrasound versus magnetic resonance imaging for deciding to proceed with uterine artery embolization for presumed symtomatic fibroids. Clin Radiol 2011;66(1):57-62.
18.- Vykliulk MV, Dedy TV: Ultrasound characteristics of uterine myoma before and after uterine artery embolization. Vestn Rentgenol Radiol. 2011; 36 (1): 18-21.
19.- Van der Kooij SM, Hehenkamp WJ, Volkers NA,Birnie E, Ankum WM,Reekers JA. Uterine artery embolization vs hysterectomy in the treatment of symtomatic uterine fibroids 5-year outcome from the randomized EMMY trial. Am J Obst Gynecol 2010;203(2):105-10.
20.- Txier H, Grevoul J, Loffroy R, et al. Uterine arteries in preparation for consecutive uterine fibroma surgery. Act Obtet Gynecol Scand. 2010;89(10):1310-1315.
21.- Hu NN, Kaw D, McCullough MF, Nsouli H,Spies JB: Menopause and menopausal symptoms after ovarian artery embolization: a comparison with uterine artery embolization controls. J Vas Interv Radiol 2010;22(5):710-715.
22.- Kim KA, Yoon SW, Yoon BS, Park CT, Kim SH, Lee JT: Spontaneous vaginal expulsion of uterine mioma after Magnetic resonance-guided focoused ultrasound surgery. J Minin Invasive Gynecol 2011;18(1):131-134.
23.- Ahn EH, Mastsuo K. Area of uncertainty in uterine arterial embolization does it increase the risk of ovarian cancer. J Obstet Gynaecol Res 2010;36(4):920.
24.- Goldberg J. Advanced ovarian carcinoma following bilateral uterine embolization. J Reprod Med 2010;55(3):179-180
25.- Pinto I, Porras J, Ayerbe E, Millan I, Bruna I, Cano ML. Pregnancy after uterine fibroid embolization: follow-up of 100 patients using tris-acryl gelatin microspheres. Fertil and Steril 2008;90(6):2356-2360
26.- Takahashi H, Hayashi S, Matsuoka K, Kitagawa M. Placenta accreta following uterine artery embolization. Taiwan J Obstet Gynecol 2010;49(2):197-198
CORRESPONDENCE:
Dr. A. Garcia-Iglesias.
Hospital Universitario de Salamanca. Departamento de Ginecología y Obstetricia.
Paseo de San Vicente nº 58.
37007 Salamanca. España
Email: aiglesias @ usal.es
Fax: (+34) 923 29 47 24
