Indice del volumen Volume index
Comité Editorial Editorial Board
Comité Científico Scientific Committee
THE DIAMNIOTIC MONOCHORIONIC (DIMO) PLACENTA ASSOCIATED TO THREE COMPLICATIONS OF THE PREGNANCY.
Olivar C. Castejon Sandoval PhD.1 Angela J López G2, Joyce Y Urdaneta Bcs. Msc.3, Stephanie Cuervo 4, Miguel Moreno 4
1Full Professor Bsc, Lic, Msc, General Director and Founder of the CIADANA(Center for Research and Analysis Assistancel Teaching of the Aragua Nucleus). Electron Microscopy Laboratory. Faculty of Health Sciences. University of Carabobo.
2Full Professor, Bsc, Lic, Msc, Last year in the Doctorate of Health Public. Deparment of Morphophysiological sciences. Bioanalysis School, Faculty of Health Sciences.
3Bsc, Lic, Msc. Electron Microscopy Laboratory, CIADANA
4Bsc, Surgeons physicians. Faculty of Health Sciences, Medicine School, University of Carabobo.
Aragua State, Maracay, Venezuela.
Email: olivar.ciadanauc @ gmail.com
Rev Electron Biomed / Electron J Biomed 2022;1:37-48.
RESUMEN
Objetivo: Reportar el caso en el cual mujer embarazada de 19 años de edad y 36 semanas de embarazo con tratamiento por sífilis fue obtenida su placenta diamniotica monocorionica también infectada por un virus desconocido y con presencia de incompatibilidad RH, siendo analizada para el estudio usando microscopía de luz.
Metodo: La placenta obtenida mediante operación de cesárea estuvo asociada a dos recién nacidos femeninos que nacieron con crecimiento discordante en peso y altura.Las dos regiones placentarias fueron descritas.
Resultados: La región placentaria del gemelo donador presentó inmadurez, fibrosis estromal, proliferación celular, cuerpos de inclusión nuclear, severo daño de la pared de los vasos y interrupciones del sincitio. El gemelo receptor estuvo asociado a región placentaria inmadura, cuerpos de inclusión intranuclear, proliferación celular, sincitio interrumpido, eritrocitos fusionados en el interior del vaso y corangiosis en la región estromal.
Conclusión: Estos resultados indican un síndrome de transfusión feto-fetal. El factor genético provocado por la incompatibilidad, la presencia de bacterias y viral actividad produjeron condiciones no favorables para el intercambio de gases y nutrientes en el árbol placentario lo cual pudo dejar secuelas en el futuro desarrollo de los gemelos.
PALABRAS CLAVE: Placenta Diamniotica-Monocorionica. Sifilis. Viral activity. Incompatibilidad RH.
ABSTRACT:
Objective: In a case report to describe that woman pregnancy of 19 years old and 36 weeks of gestation with treatment by syphilis was obtained their placenta diamniotic monochorionic also infected by a virus unknown, with presence of RH incompatibility and analysed for the study using light microscopy.
Method: The placenta in caesarean attainment was seen associate to two female newborns that had discordant growth in weight and height and their placental histological findings were descript.
Results: The win minor was conected to a region placental with immaturity, stromal fibrosis, cellular proliferation, intranuclear inclusion bodies, severe damage of the wall of the vessels and interruptions of the syncytio. The win higher also was associated to placental region of immaturity, intranuclear inclusion bodies, cellular proliferation, syncytial interruption, fusioned erythrocytes into of the vessels and chorangiosis in stromal region.
Conclusion: These results are indicating a syndrome of transfusion feto-fetal. The genetic factor provoqued by RH incompatibility, presence of bacterial and viral activity have produced conditions not favorable for the interchange of gases and nutrients in the placental tree which could to leave sequels in the future development of the wins.
KEY WORDS: Diamniotic-Monochorionic placenta. Siphylis. Viral activity. RH Incompatibility
INTRODUCTION
In the multiple pregnancies Diamniotic monochorionic (Dimo) placenta has the highest frecuency. It is considered a pathologic event, with paracentral location of the umbilical cord, histological changes as infarcts, calcifications, fibrosis, subchorionicfibrin, chorangiosis, vascular congestion and hidropic villi, besides infection changes as corionitis, deciduitis, villitis and funiculitis. The presence of unic umbilical artheria in any cases can to have relationship with fetal malformation provoqued by drugs, infections or diseases during pregnancy1.
In this case the two amniotic adjacent sacs are closing the extraembrionary space and the amnios form an interwin membrane very thin2. The fetus of this placenta are more heavy that the of monoamniotic monochorial placenta since these are associated to a gestational age minor3. This type of placenta is found into a situation hemodynamic complex with rate of mortality 2.8%, risk of premature labor and risk of RCIU4. Associate to syndrome of transfusion feto-fetal where two fetuses are connected to the placenta with deep anastomosis arterio-venous, unidirectional blood flux, donor twin and receptor twin5.
The placentation monochorionic has an ambient less favorable for the development of the fetus. The twin's diamniotic-monochorionic are of increased risks in comparison with twin dicigotic6. When occurs the death in one of these fetuses with survivor of the another in early pregnancy, the amniotic liquid is reabsorbed and the death fetus mummified is transformed in a papyraceous fetus in the syndrome of transfusion feto-fetal1. The vascular anastomosis leads to share in anormal form the fetal circulation provoquing a disbalance of the blood flux. This syndrome is found in 1/400 pregnancies and their mortality is >80% without medical treatment.30-40% of the survivors have sequels7.
In Dimo twin placenta many anastomosis can to be seen, LargeA-A anastomosis and Finer A-V in the placental thickness. With the stain of injection using bariun sulfate in this type of placenta associate to velamentous insertion of one cord, to 26 weeks gestation, the twin was connected to much smaller portion of placental tissue and died. If both cords have a marginal insertion, arteries cross over veins and there are not anastomoses. The demonstration of anastomosis is most difficult when one fetus has died before birth8.
The mortality, neonatal morbidity and birth weight disccordancy have been studied in relation to these types of anastomosis, types and distance between cord insertions and placental sharing9. But the histological aspects of the placental structure associate to the cords have not been studied equally. The angioarchitecture in monochorionic twin placenta is the principal objective in these types of placenta in relation with mortality since if mortality occurred in two fetuses usually had an arterio-arterial anastomosis; if pregnancy was complicated by one death; a venous-venous anastomosis is more likely to be present10. To describe the placenta DIMO associate to sifilis, an unknown viral activity and RH incompatibility without fetal mortality is our objective.
CASE REPORT
In woman pregnancy of 19 years old and 36 weeks of gestation with treatment by Siphilis was obtained their diamniotic monochorionic placenta also infected by a virus unknown and with presence of RH incompatibility which was analysed for the study using light microscopy.Patient was notified of the investigation and gave informed consent after the nature of procedure had been fully explained.The protocol was carried out in accordance with our institutional ethical requirements and the principles outlined in the Helsinki Declaration.The research discussed here was institutionally reviewed and approved. The presence of placental viral activity was detected after of the obtention of the placenta when the placental observations were doing with the light microscope. The placenta was obtained by caesarean section. Two female newborns were born well: NB-1 in podalic presentation, weight of 1850gr, heigt of 45cm and NB-2 in transverse position, weight of 2200gr and height of 47cm. The regions of each umbilical cord were located in the placenta and marked as A and B, these placental regions correspond with NB-1 and NB-2. 16 histological slides of the region A and equally of region B were observed and the results more rebound were described.
RESULTS
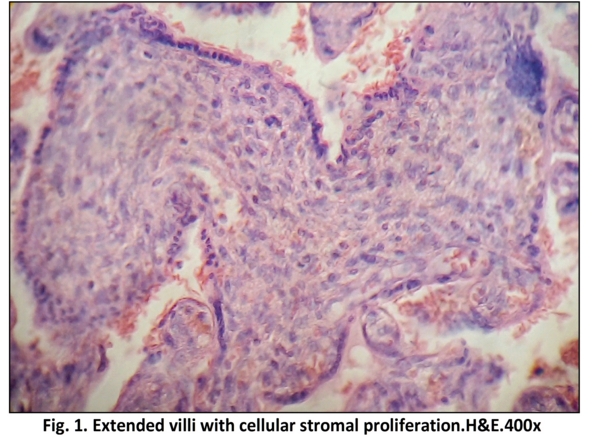
Region A. Correspond with donor win. Some placental villi appear as very broad, or thick as immature villi but without channels of Hoff Bauer, with dense stromal region formed by fibers and proliferation of cells. Diminutive vessels are noted in the peripheral region (Fig.1)
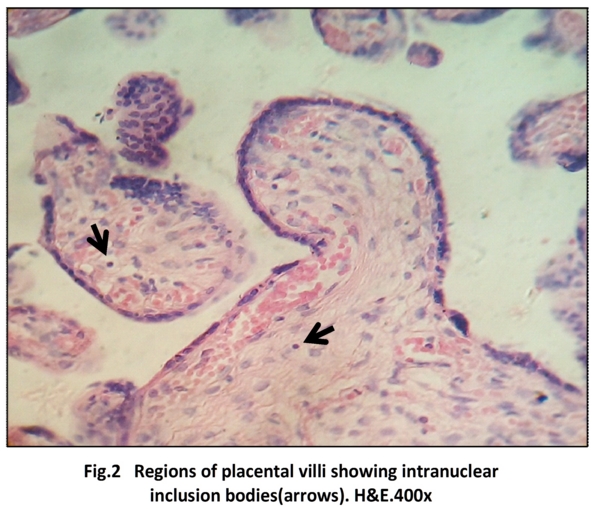
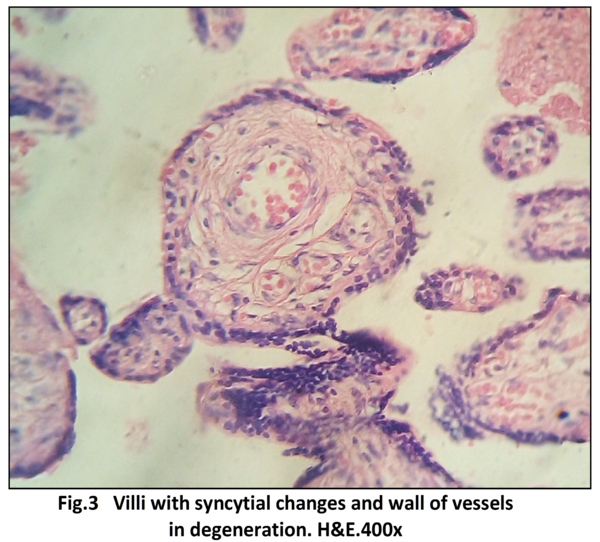
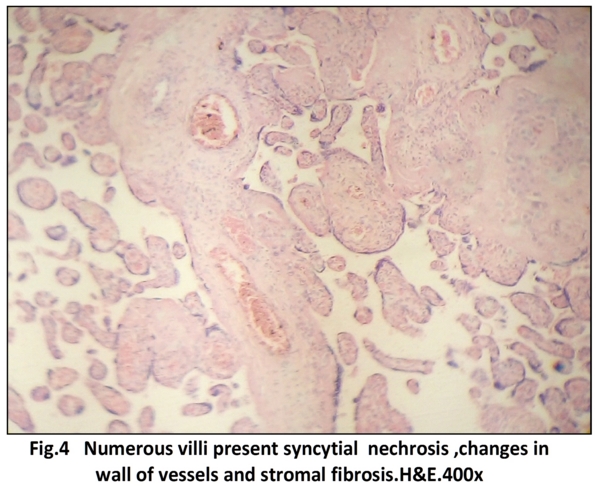
Pathognomonic intranuclear inclusion bodies, owl eye, or virocytes are observed in the stromal region (Fig.2). Severe damage in the wall of the vessels can to be observed in numerous villi (Fig3). Stem villi contain damaged vessels and there are extensive regions of villi with interruptions of the syncytio (Fig.4).
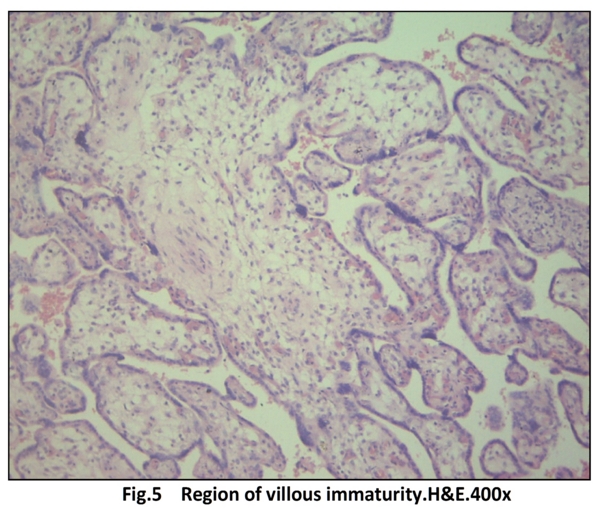
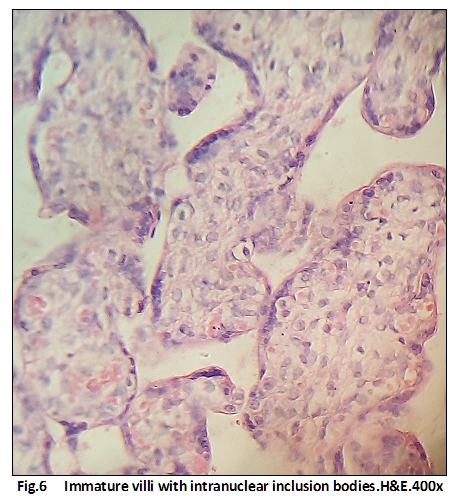
Region B. Correspond with receipt win. A numerous congregation of villi can to be observed in the which was noted the presence of intranuclear inclusions and of features of immaturity (Fig.5). In these villi the abundance of cells in the stromal region, the interruption of the syncytio and the owl eyes are remarkable the which have been indicating viral activity (Fig.6).
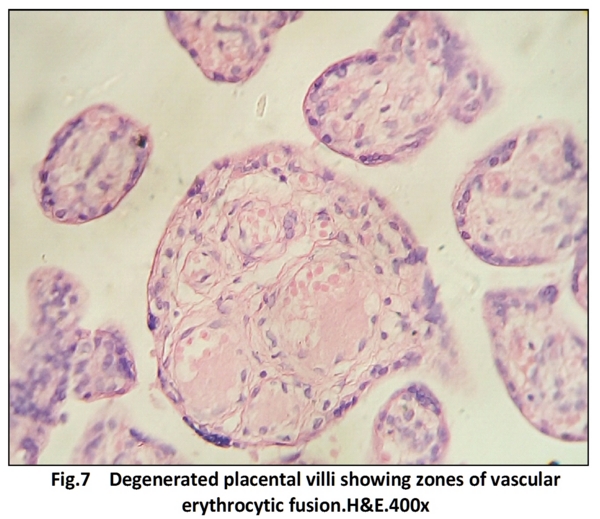
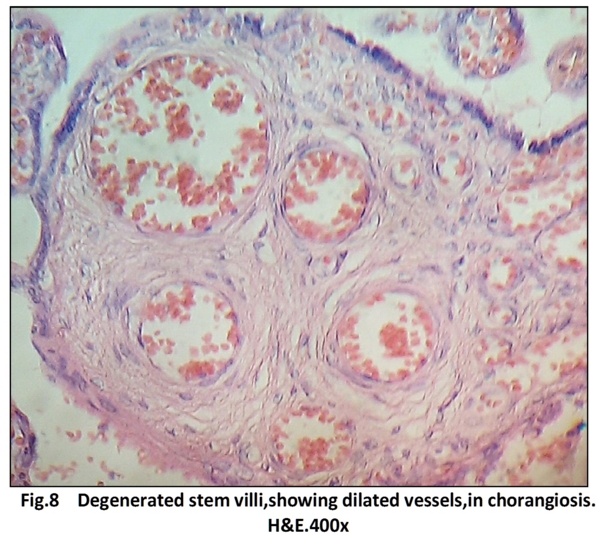
The effect of the production of maternal antibodies against antigens of fetal erithrocytes is found in degenerated villi (Fig.7). The resulting response is a placental villi in chorangiosis for to maintain the histological balance (Fig.8).
DISCUSSION
Diamniotic monochorionic twins they face increased risks because of the shared circulation, an imbalance in blood exchange occurs in anemia polycythemia sequence. Fertility treatment increases the chance from 1 in 250 to 1 in 50 after in vitro fertilization, 65% of spontaneous monocigotic twins are monochorionic. Most 85% after 32 weeks results in two healthy children and an interwin transfusion imbalance in 15%11.
The immaturity here observed is provoqued in part by RH incompatibility where the absence of proliferation of vessels, lack of any extensive regeneration of epithelial plates or the placental insufficiency caused by these changes with the existent hemolysis represents a prominent retardation of maturation12. The increase of villous stromal cells was ultrastructurally identified as produced by mesenchymal cells and Hoffbauer cells13.
The pathonogmonic intranuclear inclusion bodies are seen in bacterial infections, fungal, viral, autoimmune diseases and numerous diseases. These bodies named "Owl´eyes" are large intranuclear viral inclusion bodies with thickened nuclear membrane as noted in Hodgkin´s lymphomas. These inclusions are surrounded by a perinuclear band clear14.
The damage to the vessels here observed in stem and intermediate placental villi have been used for confirm a strong association between placental histopathologic features and congenital syphilis indicating that when such features are present, PCR of placental tissue may confirm the diagnosis of congenital syphilis15.
So, endarteritis, periarteritis, with exudates consisting of fibrin, necrotic tissue fragments and polymorphonuclear leukocytes, dense inflammatory infiltrate with lymphocytes, plasma cells and histiocytes in perivascular area is involved with endothelial-cell swelling in small blood vessels. This inflammatory exudate is followed by obliterative endarteritis of vessels and furtherly by scar tissue develops16.
The placenta of the receipt win also presented immaturity, viral activity and the syncytial interruptions. It has been mentioned that placental histological features associated with congenital syphilis include a triad of enlarged hypercellular villi, vascular changes and villitis17.
The placenta is alert to any infectious challenge, an active immune-mechanical barrier protects against viral infections, the syncytio acts as a source of immune molecules such as antimicrobial peptides ,activation of dendritic cells, a pro-inflammatory responses by peripheral natural killer cells and monocytes, the syncytio possess hight rates of basal autophagy and others mechanisms of defense18.
The pathophysiology of RH incompatibility indicate that when a RH-negative mother is exposed to the RHD antigen of their fetus it is perceived as a foreign threat and she produces anti-D antibodies which are bind to the D antigen present on the fetal erythrocytes provoquing their hemolysis19.
The identification of trasplacental haemorrhage as the stimulus for anti-D antibody production led to the development of anti-D immunoglobuling prophylaxis for RHD negative women who are not alloimmunised. Prevention includes administration of anti-D immunoglobulin at 34 weeks of gestation at delivery of an RHD positive infant20.
In these types of placenta there is placental share discordance or unequal placental sharing and vascular anastomosis. The unidirectional blood flow in arterio-arterial anastomosis enables volume disequilibrium, resulting in severe complications such as syndrome of transfusion in monochorionic twins (TTTS) leading to discordant fetal growth and selective intrauterine growth restriction21.
These studies have been possible with careful placenta examination and injection technique with colored dye. Selective intrauterine growth restriction (sIUGR) affects to 10-20% of monochorionic twin pregnancies and is strongly associate with unequal placental sharing. A large placental share for the larget twin and a small placental share for the growth restricted twin. The velamentous cord insertion belong usually to the growth restricted fetus22.
The genetic factor provoqued by the incompatibility, the presence of bacterial and viral activity have produced conditions not favorable for the interchange of gases and nutrients in the placental tree. It can to give origin to fetal death. Besides, could to leave sequels in the future development of the wins. Nevertheless the majority of DiamnioticMonochorionic pregnancies are viable.
REFERENCES
1.- Gonzalez MLC, Paiva S. Embarazo multiple; estudio de sus placentas. Rev Obstet Ginecol Venez 2009;69(4):226-230.
2.- Gil GED, Gil MEG. Diagnostico ecográfico de la corionicidad y amnionicidad en el embarazo multiple .Rev Per Ginecol Obstet 2015;61(3):263-268.
3.- Dicastro P. El embarazo múltiple. Aspectos anatomopatologicos. Perinatol Reprod Hum 1997;11(2):1-99.
4.- Machin G, Still K, Lalani T. Correlations of placental vascular anatomy and clinical outcomes in 69 monochorionic twin pregnancies. Am J Med Genet 1996;61:229-236.
5.- Wee LY, Fisk NM. The twin-twin transfusion syndrome. Semin Neonatol 2002;7(3);187-202.
6.- Mauad F, Righi P, Silva D et al. Importancia del diagnostic temprano de la corionicidad en la gestacion gemelar. Rev Latin Perinat 2019;22(1):58-62.
7.- Sebire NJ, Snijders RJ, Hughes K et al. The hidden mortality of monochorionic twin pregnancies. Br J Obstet Gynecol 1997; 104:1203-1207.
8.- Benirschke K, Kaufmann P. Pathology of the Human Placenta. Fourth Edition 2000; New York: Springer-Verlag; pp805-808.
9.- Hack KEA, Nikkels PGJ, Koopman EC et al. Placental characteristics of Monochorionic Diamniotic twin pregnancies in relation to perinatal outcome. Placenta 2008;29(11):976-981.
10.- Nikkels PGJ ,Hack KEA, vGemert MJC. Pathology of twin placentas with special attention to monochorionic twin placentas. J Clin Pathol 2008;61(12):1247-1253.
11.- Lewi L. Monochorionic diamniotic twins: what do I tell to the prospective parents? Prenat Diagn 2020; 40:766-775.
12.- Stoz F, Keckstein G, Schuhmann RA. Histometric case report of a placenta following intra-uterine therapy of rhesus incompatibility. Geburts hilfe Frauenheilkd 1987;47(5):349-350.
13.- Walter P, Blot P, Ivanoff B. Tha placental lesions in congenital syphilis. A study of six cases. Virchow Arch A Pathol Anat Histol 1982;397(3):313-326.
14.- Balachander N, Rajesh E, Priya SH et al. Inclusion bodies. Biomed Pharmacol J 2016;9(2)
15.- Genest DR, Choi-Hong SR, Tate JE et al. Diagnosis of congenital syphilis from placental examination: Comparison of histopathology, steiner stain, and polymerase chain reaction for Treponema pallidum DNA. Hum Pathol 1996;27(4):366-372.
16.- Singh AE, Romanowski B. Syphilis; Review with emphasis on clinical, epidemiologic and some biologic features. Clin Microbiol Rev 1999;12(2):187-209.
17.- Zaga CV, Diaz L, Olmos OA et al. Central role of the placenta during viral infection: immune-competences and RNA defensive responses. Bioch Biophy Act Mol Bas Dis 2021;1867(10):166-182.
18.- Costumbrado J, Mansour T, hassemzadeh S. RH Incompatibility. Stat Pearls (Internet). Treasure Island(FL): Stat Pearls Publishing 2021.
19.- Urbaniak SJ, Greiss MA. RHD haemolytic disease of the fetus and the newborn .Blood Rev 2000;14(1):44-61.
20.- Zhao D, Lipa M, Wielgos M et al. Comparison between monochorionic and dichorionic placentas with special attention to vascular anastomosis and placental share. Twin Res Hum Gen 2016;19(3):191-196.
21.- Zhao D, de Villiers SF, Oepkes D et al. Monochorionic twin placentas: Injection technique and analysis. Diagn Prenat 2014;25(2):35-42.
CONFLICTS OF INTEREST
The authors declare that they had no funding to carry out this study and that there are no conflicts of interest to declare.
CORRESPONDENCE:
Prof. Olivar Clemente Castejon Sandoval
Director of the Center for Research and Analysis Assistancel Teaching of the Nucleus Aragua (CIADANA).
Electron Microscopy Laboratory.
Faculty of Health Sciences. University of Carabobo. Aragua Nucleus.
Aragua State.
Maracay, Venezuela.
Email: olivar. ciadanauc @ gmail.com
Recibido 14/02/2022.
Publicado 15/02/2022